Why skipping antidepressant doses is a risky way to taper
A Reader’s Digest version of our new paper
For years, many doctors have advised patients who want to come off antidepressants to simply “take your pill every other day for a while.”
It sounds sensible: you’re reducing your “average” dose, right?
But here’s the problem. Skipping doses throws your brain chemistry on a rollercoaster. And our new study in the Journal of Affective Disorders shows just how steep and risky those ups and downs can be.
What we wanted to know
In my practice, I’ve seen countless people try to follow this advice (before they’ve learned about the principles of hyperbolic tapering, that is). Almost every time, it goes badly. People report dizziness, anxiety, inner restlessness, insomnia, intrusive thoughts, brain zaps, and otherwise unexplained low mood. But the advice keeps getting passed down.
We asked: What’s really happening in the brain when people “taper” by skipping days?
What we did
Together with colleagues in the UK, we modeled what happens in the brain when you take antidepressants daily versus every other or third day.
We ran computer simulations (“in silico modeling”) of five common antidepressants: citalopram, escitalopram, sertraline, duloxetine, and mirtazapine.
We tracked how drug plasma levels rise and fall in the body and how that affects the brain receptors these drugs act on (primary receptor occupancy).
What we found
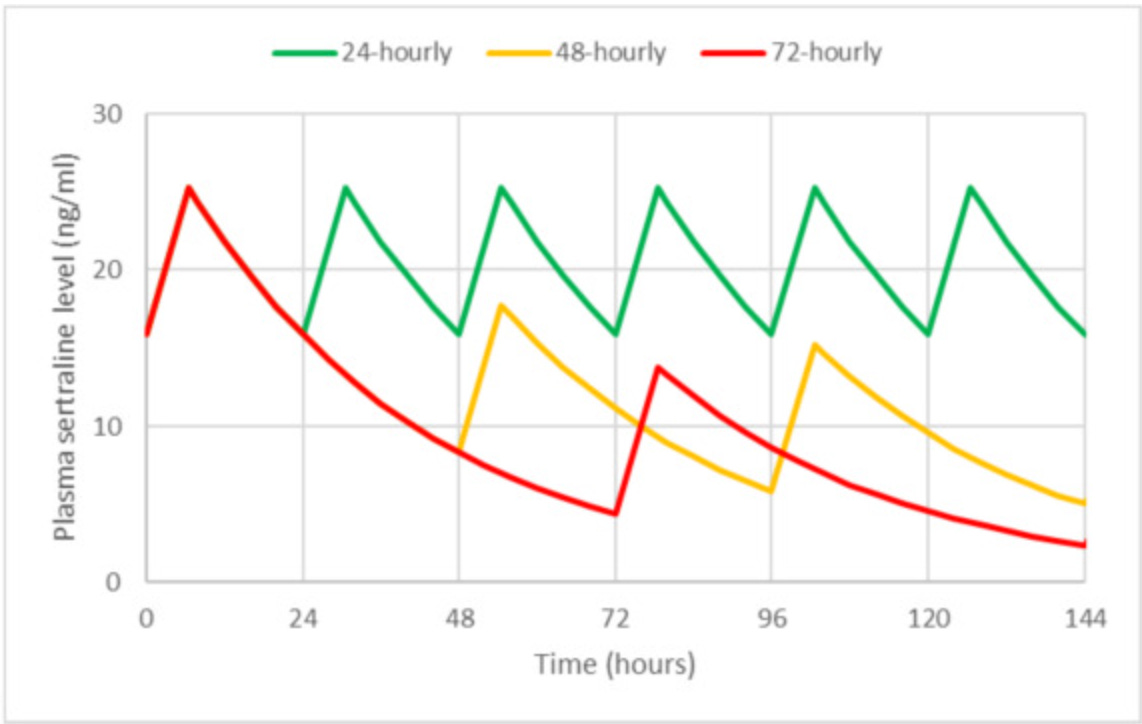
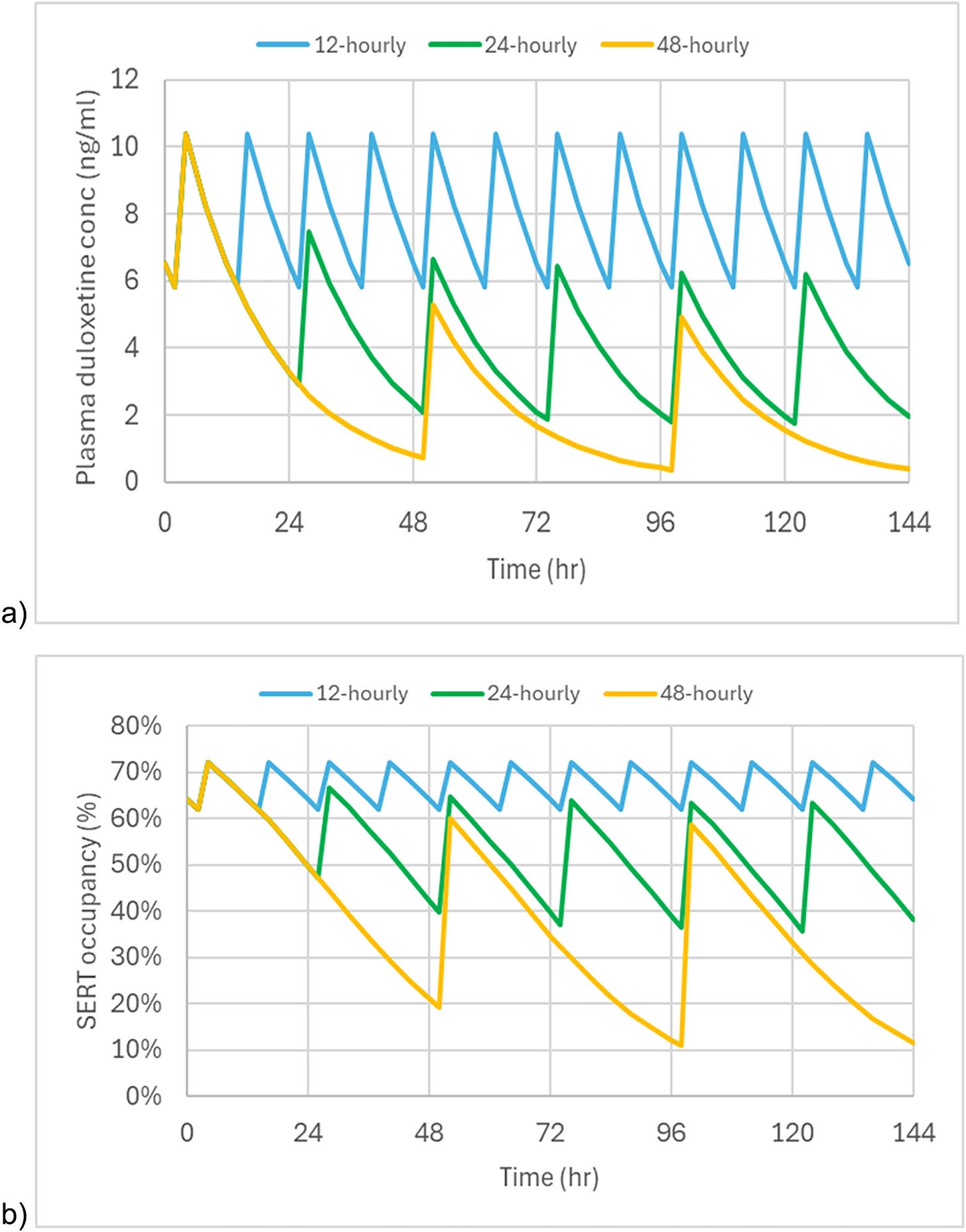
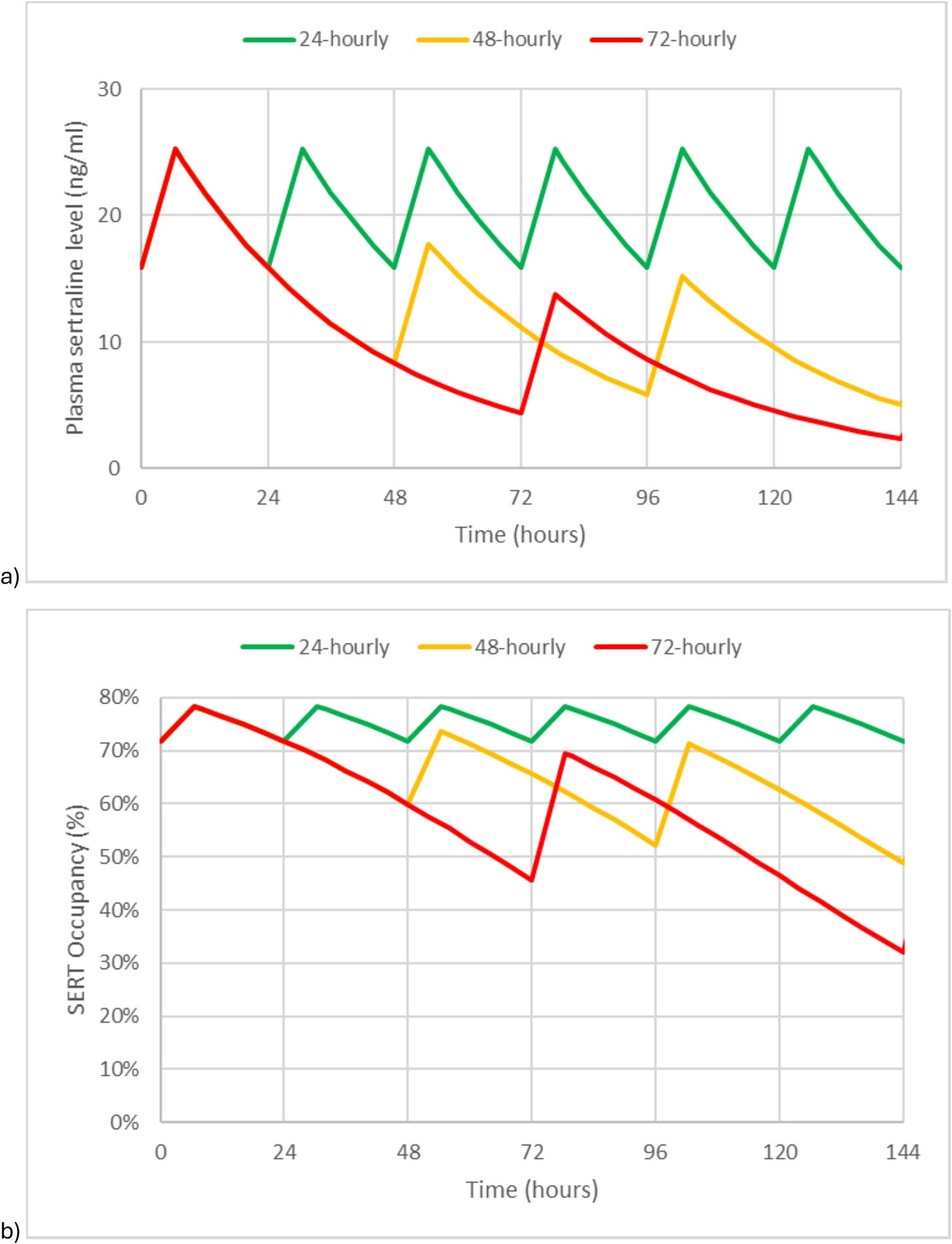
… is best illustrated:
Clearly, skipping doses makes drug levels swing up and down dramatically, while taking daily doses ensures relatively steady levels (although a drug is technically never constant in the body).
Those swings:
1) Were 2x to 5x larger when skipping days,
2) Grew worse at lower doses (ironically, the stage when people are most vulnerable to withdrawal)
3) Are exactly the kind of instability known to trigger withdrawal symptoms.
Why this matters
When people are tapering a psychiatric drug, they’re already navigating a fragile transition. The last thing they need is instability in the brain’s chemistry.
As we’ve talked about here before, the whole point of tapering - instead of just stopping - is to give the brain and body time to gradually adapt to less and less of the drug. But if a higher dose suddenly hits the system every second or third day anyway, that adaptation to the lower dose never happens.
Put simply, homeostasis can’t do its thing if we keep giving the brain mixed signals. Our nervous system is a lazy but clever organism - always trying to predict what’s coming next. If the input keeps changing, it gets confused, and withdrawal is often the result.
Yet the advice to skip doses is still widespread. I see it in guidelines, and I hear it from patients nearly every week. And while psychiatry has a long track record of being resistant to evidence, I hope this paper will help put an end to this particular piece of harmful advice.
Antidepressant withdrawal is already difficult enough. Outdated tapering advice can make it outright unbearable, sometimes forcing people back on medication when they might have succeeded with a safer approach.
A better way
If you’re coming off antidepressants, don’t skip doses. It’s not a safe shortcut. It’s not a smart alternative to the nitty-gritty work of a proper hyperbolic taper. It increases the risk of severe withdrawal. And maybe most importantly, it offers no advantage whatsoever over doing the taper properly.
Use smaller daily doses instead; through liquid formulations, counting beads, tapering strips, or compounded medication. This approach keeps brain chemistry more stable on its way down to zero and lowers the risk of severe withdrawal.
I go deeper into these strategies in my book, Crossing Zero: The Art and Science of Coming Off – and Staying Off – Psychiatric Drugs. And if your doctor resists, point them to this paper or to The Maudsley Deprescribing Guidelines by Mark Horowitz and David Taylor - both co-authors here, and the most credible resource available for doctors.
And here’s a twist our modeling revealed: for drugs with shorter half-lives (like duloxetine and sertraline), taking them twice a day instead of once daily could actually make tapering smoother - especially when reaching the lower dose range. It’s the opposite of what people are usually told, but it makes perfect sense: the steadier the brain chemistry, the easier the transition. How to actually spread the dose from once- to twice-daily without triggering withdrawal is a bigger topic, and one we’ll save for another article if readers are interested.
That’s it for today. Stay tuned for my next post on Tuesday - a guest piece in Roger McFillin’s Substack, Radically Genuine, which I highly recommend.
This article is based on our new paper in the Journal of Affective Disorders:
“Alternate-day dosing to taper antidepressants risks severe withdrawal effects: an in silico analysis.”Grateful to James O’Neill, David Taylor, and Mark Horowitz for inviting me to co-author this paper. Be sure to follow these guys for more excellent research!



Definitely interested in more info about spreading doses as a way to maybe taper more gently from AD’s like Paxil (I’m stuck on 3mg…).
Grateful for all the work you’re doing!
It would very helpful to have a follow up article to this for those of us who have been told by our doctors to skip doses and now find ourselves in horrendous withdrawal, how do we remedy that in order to stabilise our system thanks